 What is a cataract?
What is a cataract?
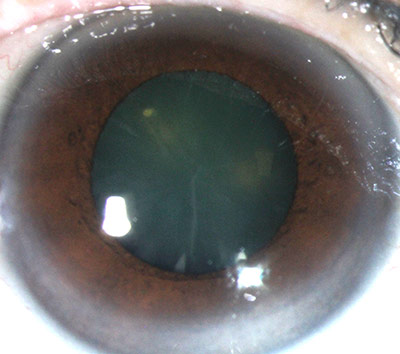
Cataract refers to the clouding of the natural lens of the eye. This occurs with aging, but may occur earlier in some people (e.g. diabetics, patients on long-term steroid use).
How do I know if I have cataract(s)?
Patients may notice slowly progressive, painless blurring of vision. One eye may be more affected than the other. Some people may also experience increased glare, dimming of vision, and loss of color brightness.
Can cataract be prevented?
There is no known prevention for age-related cataract. However, reducing sunlight exposure (ultraviolet rays) may slow down its progression.
What happens if I leave my cataract(s) untreated?
Cataract(s) cause gradual loss of vision and ultimately blindness if left untreated. In unusual situations, it may lead to a sudden increase in eye pressure that causes severe eye pain.
What treatment is available for cataract?
Early cataract(s) can be observed, and patients are usually prescribed glasses to aid their vision. When cataract(s) affects one’s vision considerably, surgical removal of the lens (cataract extraction surgery) is advised.
When should cataract(s) be removed?
Cataract surgery is recommended when the blurring of vision affects daily activities.
How is cataract surgery performed?
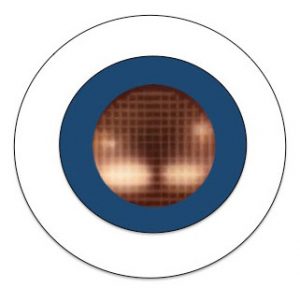
 Cataract surgery involves removing your existing lens and replacing it with an artificial intraocular lens (IOL) with refractive power correction.
Cataract surgery involves removing your existing lens and replacing it with an artificial intraocular lens (IOL) with refractive power correction.
The most common form of cataract surgery is phacoemulsification. This uses ultrasound energy to break up the lens and can be performed under local anesthesia.
In some situations where patients have more advanced cataract, they may undergo extracapsular cataract extraction (ECCE). This surgery requires a larger incision and stitches to close the wound and would therefore take longer. Vision will take longer to recover as stitches may need to be removed about one to two months after surgery.
Cataract surgery is done as a day surgery procedure. Patients are usually discharged home on the same day, a few hours after surgery. They would be started on an eye drop and reviewed in the clinic one day, one week, and one month after the operation.
After the operation, patients are given an eye shield to be used when sleeping. Patients are advised not to rub their eyes and to keep their operated eye clean and dry.
What are some important information my surgeon may need?
- You MUST inform your surgeon if you had laser refractive surgery performed (i.e. LASIK, PRK, epi-LASlK, SMILE) previously. Please bring along records of your previous treatment. This information is very important in ensuring accurate IOL calculation.
- You will need to stop wearing contact lens (at least one week for soft lens and at least two weeks for hard lens) prior to undergoing IOL calculation for surgical planning.
Can cataract surgery be done with laser?
 In femtosecond laser-assisted cataract surgery (FLACS), a precise laser substitutes some, but not all, steps of standard phacoemulsification. The laser creates an opening in the anterior lens bag, and softens the lens nucleus. It aims to reduce damage to the inner surface of the cornea and increase accuracy of intraocular lens location.
In femtosecond laser-assisted cataract surgery (FLACS), a precise laser substitutes some, but not all, steps of standard phacoemulsification. The laser creates an opening in the anterior lens bag, and softens the lens nucleus. It aims to reduce damage to the inner surface of the cornea and increase accuracy of intraocular lens location.
The laser is first performed at a separate machine, before the patient is transferred to the surgical bed for completion of the rest of the cataract surgery. Your surgeon will need to evaluate your suitability for this procedure

What is the difference between laser-assisted cataract surgery and LASIK?
LASIK treats the cornea and is used to correct refractive errors e.g. myopia. LASIK does not treat the natural lens or cataract.
Is FLACS safer than standard phacoemulsification?
FLACS reduces the average ultrasound energy delivered compared to standard phacoemulsification by 4 -8% and may cause less damage to the inner surface of the cornea.
However, in a patient with a typical cataract, there may be no added benefit to the patient’s visual outcome, and most surgeons would use standard phacoemulsification and only select femtosecond laser if patient’s eye condition truly requires it.
Would I see better after FLACS compared to phacoemulsification?
Many studies have been performed to show that the visual outcome and success rate with the use of FLACS is not better than standard phacoemulsification.
What are the risks of FLACS?
Risks include an incomplete opening in the anterior lens bag, which increase the risk of the back of the lens bag breaking and affecting the positioning of the IOL. After the surgery, there may be swelling of the back of the eye (macula edema) or high eye pressure.
Who should consider FLACS?
FLACS may be helpful for patients with less healthy corneas; it is not currently recommended as a standard procedure for all cataract surgeries.
To schedule an appointment or to know more about cataract surgery, please call 6777 6058. Alternatively please send us an enquiry.
